Specific learning objectives
- Time line of COVID-19
- Epidemiological triad
- R0/Serial interval
- Corona virus survival
- Contact
- Super spreaders
- PHEIC
- Herd immunity
- Quarantine/Isolation
- Dead body handling
- Aarogya Setu
- National sero surveillance
- Levels of prevention
- Epidemic Diseases Act, 1897
- MCQs
Introduction
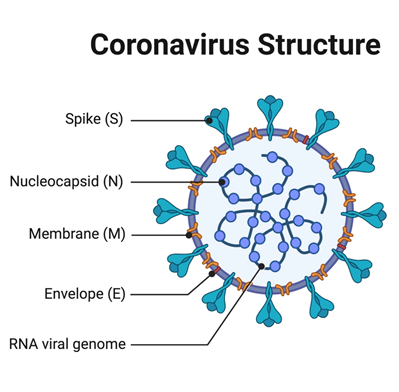
- Coronavirus are a large family of viruses causing illness in humans and animals.
- Ranging from common cold to severe diseases like MERS (Middle east respiratory syndrome), SARS (Severe acute respiratory syndrome).
- Most recently discovered nCoV (2019-2020) causes Covid19.
- Orgin: Wuhan, Hubei China.
SARS/MERS/COVID-19
- SARS – CFR: 10%
- MERS – CFR:34%
- COVID-19 – CFR: 1.5-3%
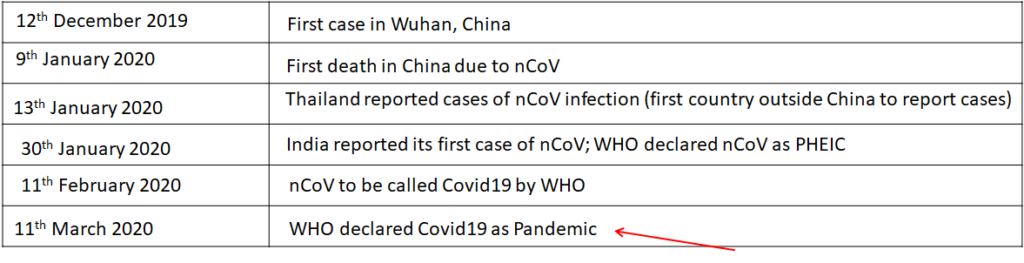
Timeline of Covid19
The epidemiological triad of nCoV 2019
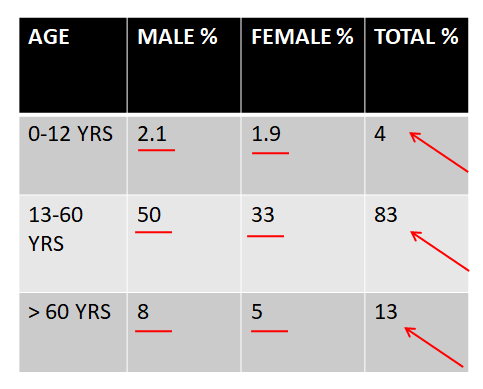
Case distribution
Epidemiology
Agent: Novel Coronavirus (pre called SARS CoV-2)
Source of infection: Cases
Mode of transmission: Droplet, Contact, Fomites
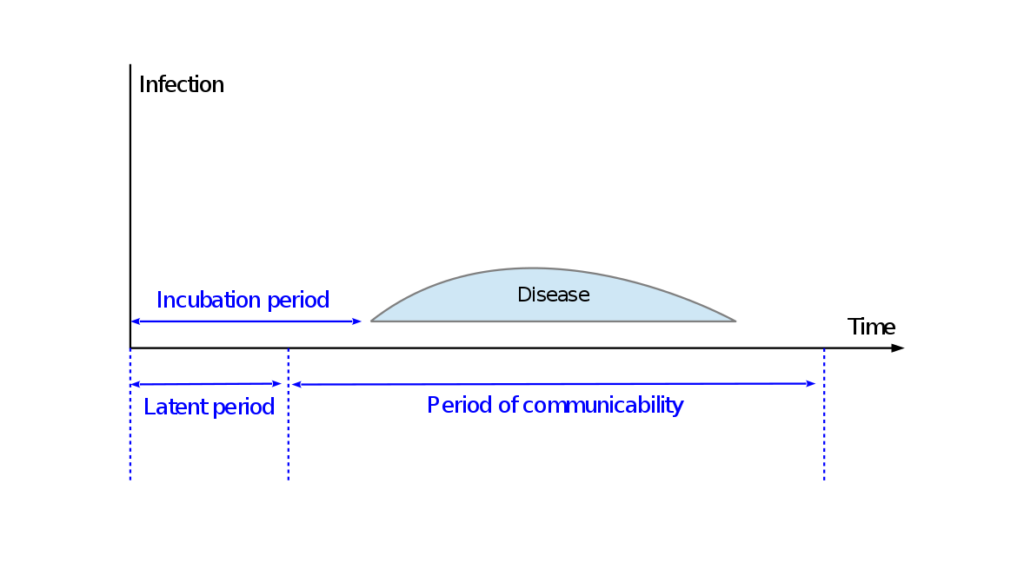
Incubation period: 2-14 days
Median incubation period: 5 days
Case fatality rate(CFR): 3% globally (India: 1.62%)
Age group affected: All age groups (mostly 30+)
CFR is highest with existing co-morbidities (CVD,HT,DM, Cancer, Chronic respiratory disease)
What is serial interval?
The serial interval is the duration between symptom onset of a primary case and symptom onset of secondary cases (contacts) generated by the primary case.
Median serial interval is about 4.0 days
<<<< median incubation period (6.0 days)
Interpretation: Super spreader
The term was first used by British physician William Pickles, who had initially referred to it as transmission interval with reference to a hepatitis epidemic in the United Kingdom during 1942-45.
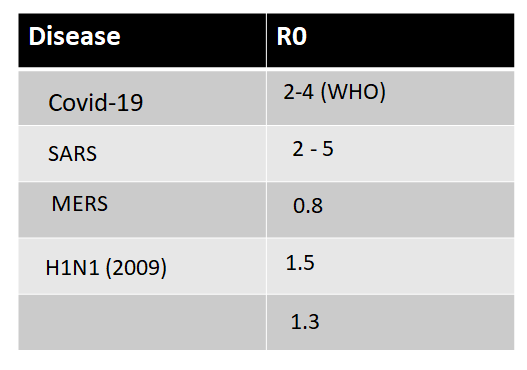
How contagious?
- R0 (R naught)
- Basic reproduction number
- An indicator how contagious is a disease
- A mathematical term that indicates how many people each infected person will in turn infect, in a fully susceptible population.
- India 1.83 (mar);1.55 (apr); 1.23 (may).
- If R0 is less than 1, each existing infection causes less than one new infection. = elimination
- If R0 equals 1, each existing infection causes one new infection. = endemic
- If R0 is more than 1, each existing infection causes more than one new infection. =epidemic.
CDC estimates of COVID-19 epidemiology parameters
- Overall symptomatic case hospitalization rate: 3.4%
- Asymptomatic SARS-CoV-2 infection rate: 35%
- Infectiousness of asymptomatic individuals relative to symptomatic individuals: 100%
- Percentage of transmission occurring prior to symptom onset: 40%
- Time from exposure to symptom onset: Mean of 6 days
Mode of Transmission
- Primarily via respiratory droplets – person to person – in close contact (usually within about 6 feet).
- Infected droplets >5micron travel <1m
- <5micron 1m to 2m only
- Virus released in respiratory secretions (eg, during coughing, sneezing, talking) can infect other individuals via contact with mucous membranes.
- Contact with fomites is thought to be less significant than person-to-person spread as a means of transmission.
Inanimate objects
Air: 3 hours
Copper surfaces: 4 hours
Cardboard: upto 24 hours
Stainless steel: upto 2-3 days
Polypropelene plastic: 3 days
- The virus can be effectively inactivated by surface disinfection such as
- 70% isopropyl alcohol
- 0.5% hydrogen peroxide
- or 0.1% sodium hypochlorite
Based on the evidence from New England journal of medicine
Case classification
Possible case:
Any person meeting the clinical criteria
Probable case:
Any person meeting the clinical criteria with an epidemiological link
OR
Any person meeting the diagnostic criteria
Confirmed case:
Any person meeting the laboratory criteria
- Effective contact
- Close contact
- Casual contact
- Contact tracing
Effective contact
- It is defined as anyone that a Covid patient has hugged or shook hands or spent 15 minutes within < 6 feet distance.
Casual contact definition
Casual contact is defined as any person having less than 15 minutes face-to-face contact with a confirmed case in any setting, or sharing a closed space with confirmed case for less than 2 hours.
This will include healthcare workers, other patients, or visitors who were in the same closed healthcare space as a case, but for shorter periods than those required for a close contact.
A close contact is defined as requiring greater than 15 minutes face-to-face contact with a confirmed case in any setting, or the sharing of a closed space with a confirmed case for a prolonged period (e.g. more than 2 hours).
- 1. Living in the same household or household-like setting (e.g. in a boarding school, university accommodation or hostel)
- Direct contact with the body fluids or laboratory specimens of a case without recommended PPE
- A person who spent 2 hours or longer in the same room (such as a GP or ED waiting room)
- A person in the same hospital room when an aerosol generating procedure is undertaken on the case, without recommended PPE
- Aircraft passengers who were seated in the same row as the case, or in the two rows in front or two rows behind a confirmed 2019-nCoV case.
- Contact tracing of people who may have had close contact on long bus or train trips should also be attempted where possible, using similar seating/proximity criteria.
- All other passengers are not considered to be close or casual contacts and do not require contact tracing.
- Face-to-Face contact for more than 15 minutes with the case in any other setting not listed above.
Contact tracing
- Contact tracing for COVID-19 requires identifying persons who may have been exposed to COVID-19 and following them up daily for 14 days from the last point of exposure.
- When systematically applied, contact tracing will break the chains of transmission of an infectious disease and is thus an essential public health tool for controlling infectious disease outbreaks.
Surveillance objectives
- Early identification
- Isolation of suspected and diagnosed cases
- Contact tracing and monitoring
- Collection of clinical data
- Collection of biological samples
- Regional and National diagnostic criteria
- Expert treatment consensus
- Establishment of isolation ward
- 14 days quarantine
PHEIC Public health emergency of International concern
An extraordinary event which is determined to constitute a public health risk to other States through the international spread of disease and to potentially require a coordinated international response
Criteria for PHEIC
- Public health impact
- Unusual or Unexpected cases
- High risk for international travelers
- It is a “call to action” and “last resort” measure.
Since 2009, there have been six PHEIC declarations:
1.2009 H1N1 (or swine flu) pandemic
2.2014 polio declaration
3.2014 outbreak of Ebola in Western Africa
- 2015–16 Zika virus epidemic
5.Kivu Ebola epidemic
6.2020 novel corona virus outbreak.
- The recommendations are temporary and require reviews every three months.
Criteria for PHEIC
- Public health impact
- Unusual or Unexpected cases
- High risk for international travelers
- It is a “call to action” and “last resort” measure.
Since 2009, there have been six PHEIC declarations:
1.2009 H1N1 (or swine flu) pandemic
2.2014 polio declaration
3.2014 outbreak of Ebola in Western Africa
- 2015–16 Zika virus epidemic
5.Kivu Ebola epidemic
6.2020 novel corona virus outbreak.
- The recommendations are temporary and require reviews every three months.
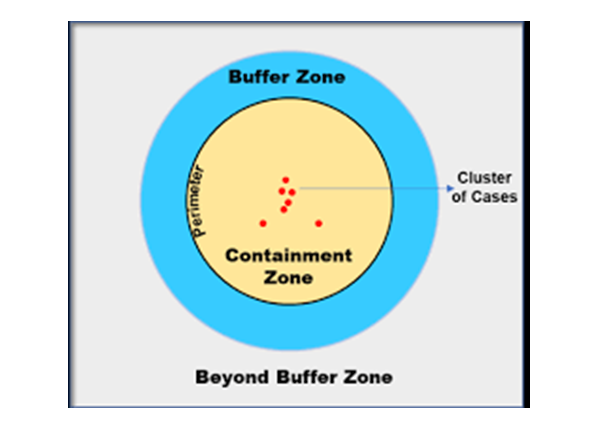
a) Sporadic cases refers to a small number of cases (one or more) that are either imported or detected locally;
b) Clusters of cases refers to cases that are clustered in time, geographic location and or by common exposures;
c) Community transmission refers to larger outbreaks of local transmission that can be defined through different approaches, including big numbers of cases not linkable to transmission chains and multiple unrelated clusters in several areas.
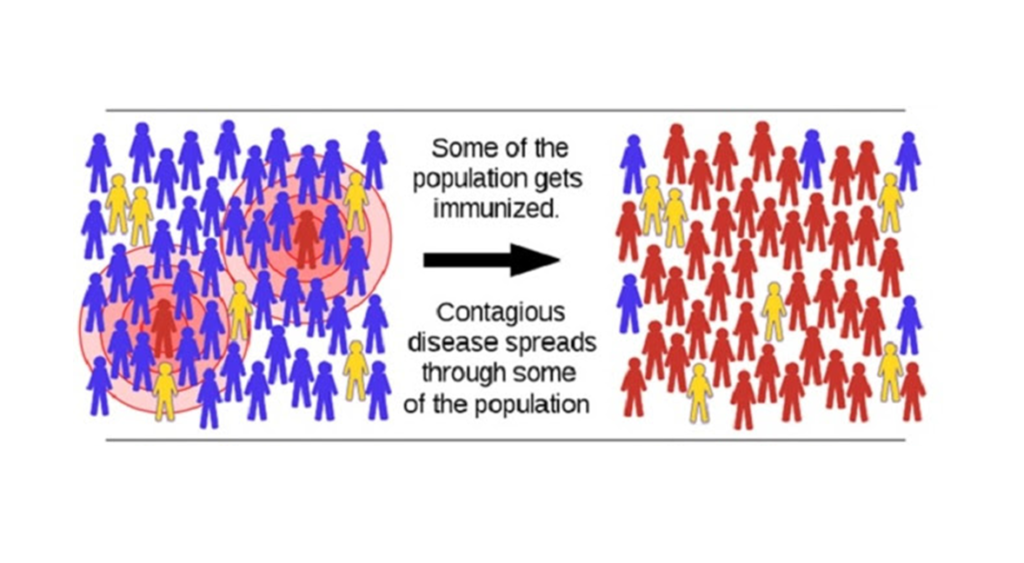
- Containment zone in cluster cases 3 km radius of primary case.
- Buffer zone is 5 km radius of primary case in cluster containment strategy of covid-19
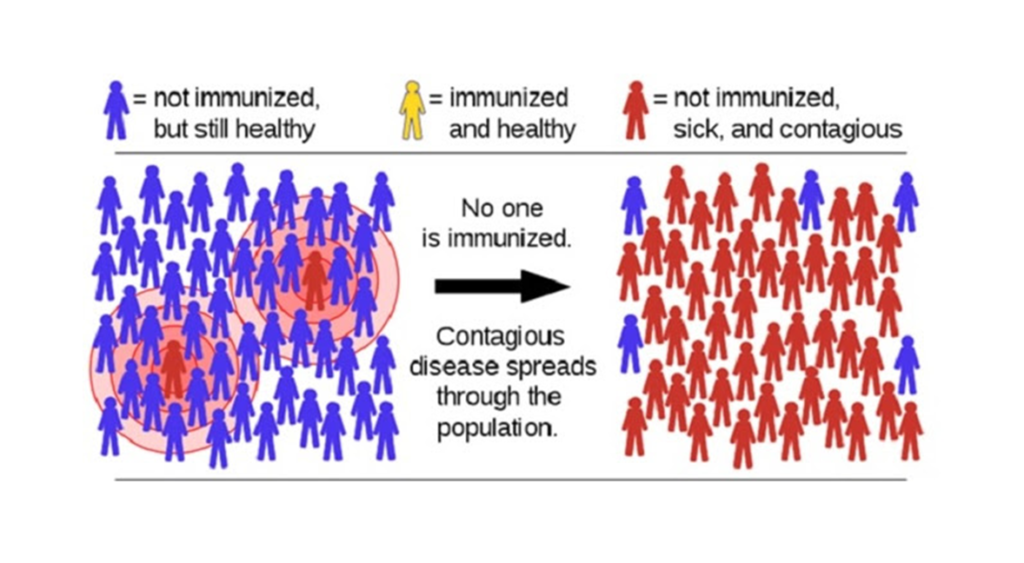
What is herd immunity? /Social vaccine
- When most of a population is immune to an infectious disease, this provides indirect protection—or herd immunity (also called herd protection)—to those who are not immune to the disease.
- For example, if 80% of a population is immune to a virus, four out of every five people who encounter someone with the disease won’t get sick (and won’t spread the disease any further). In this way, the spread of infectious diseases is kept under control. Depending how contagious an infection is, usually 50% to 90% of a population needs immunity to achieve herd immunity.

What will it take to achieve herd immunity with SARS-CoV-2?
- Here are two ways to achieve herd immunity:
- A large proportion of the population either gets infected or gets a protective vaccine.
QUARANTINE
- Separation of individuals who are not yet ill, but have been exposed to COVID-19 (i.e., have potential to become ill)
- There is voluntary home quarantine of contacts of suspect/confirmed cases, but they may also be quarantined in community-based facilities.
ISOLATION
- Separation of individuals who are ill and suspected or confirmed of COVID-19.
- Persons testing positive for COVID-19 will remain to be hospitalized till 2 of their samples test negative
Patient care in Quarantine ward
- 14 days from the time of exposure.
- Separate beds with 1- 2 meters distance, no bed facing another.
- Washable items needs to be placed in 1% hypochlorite up to 30 minutes and later washed in detergent.
- Discharged at the end of 14-day incubation period, provided the samples are negative on resampling.
- Written instructions to patients to self-monitor their health at their home (home quarantine) for the next 14 days and
- District and state surveillance units should be given contact details of the quarantined people to conduct active surveillance for the next 14 days and intimate it to the central surveillance unit, idsp (ncdc).
Patient care in isolation ward
- Patients housed in single rooms. If single rooms not available, beds put at a distance of at least 1 meter (3 feet).
- Adequate room ventilation: If air-conditioned, 12 air changes per hour + filtering of exhaust air.
- If air-conditioning not available, negative pressure created through 3-4 exhaust fans to drive air out. [negative pressure rooms with minimum of 12 air changes per hour or at least 160 litres/second/patient in facilities with natural ventilation]
- If sufficient room space, have natural ventilation – large windows on opposite walls allowing unidirectional flow and air changes.
- Telephone or other communication method in the room to enable visitors to talk with healthcare workers to reduce the number of times the workers need to don PPE to enter the isolation area.
Cleaning/decontamination needs to be performed using the proper PPE and adopting the three-bucket system
- First mop the accessible surfaces with warm water and detergent solution.
- After mopping, clean the mop in plain water (Change the water when dirty).
- After drying, mop the area using 1% sodium hypochlorite working solution
- Followed by cleaning with a neutral detergent for removing the traces of the hypochlorite solution.


Dead body handling
- Plug Oral, nasal orifices of the dead body to prevent leakage of body fluids
- Place the dead body in leak-proof plastic body bag.
- The exterior of the body bag can be decontaminated with 1% hypochlorite.
- The body bag can be wrapped with a mortuary sheet or sheet provided by the family members.
- Bathing, kissing, hugging, etc. of the dead body should not be allowed. other last rites that does not require touching of the body can be allowed
- The ash does not pose any risk and can be collected to perform the last rites
Aarogya Setu

- Covid19 tracking mobile application (National Information centre ) under Ministry of Electronics and Information technology.
- Awareness among general population
- Risk assessment (self)
- Cases among our vicinity
- All India National helpline for Covid19 (24*7) is 1075
National Sero-surveillance
- Sampling strategy: The districts will be categorized into four strata according to the reported COVID-19 cases per million population (zero, low: 0.1-4.7, medium: 4.8-10 and high: >10).
- Fifteen districts from each stratum will be selected randomly for a total of 60 districts.
- In addition, the top 10 cities reporting the highest number of cases in the country will be included, to be considered as hotspots.
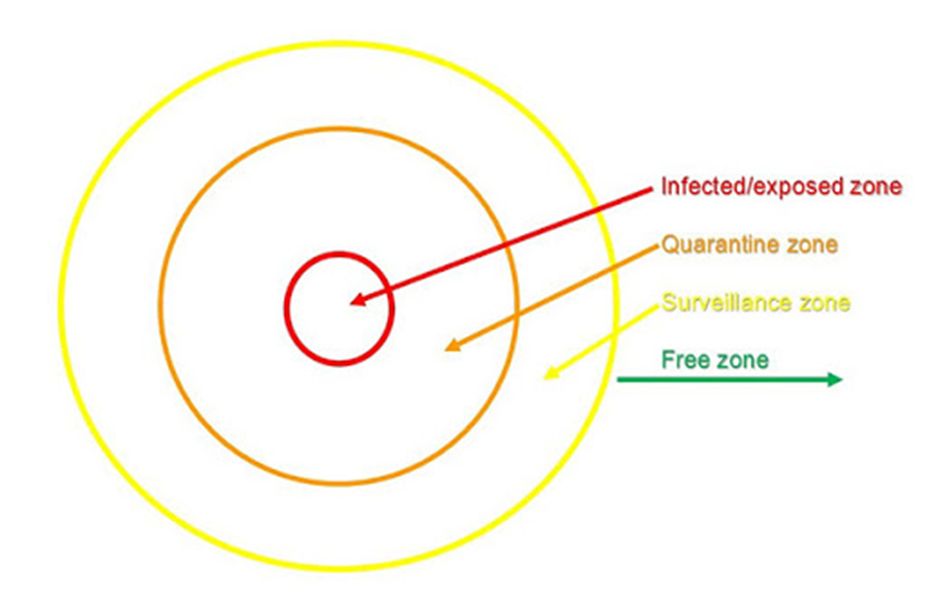
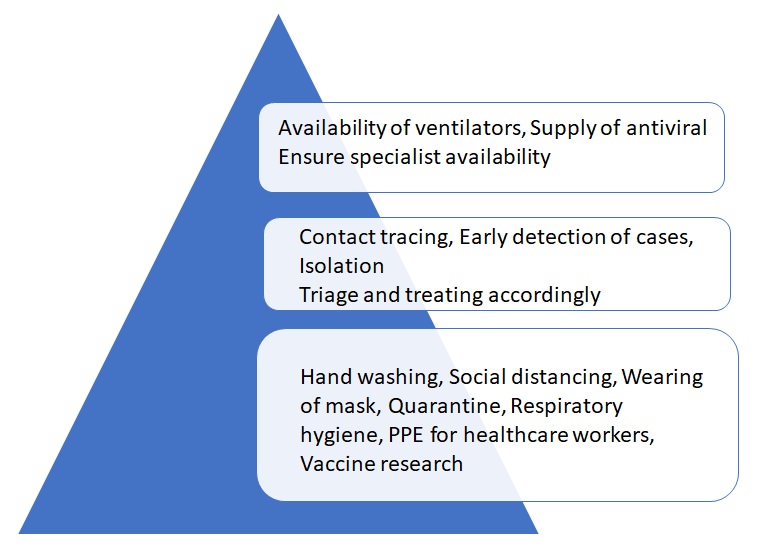
Levels of prevention
Levels of prevention
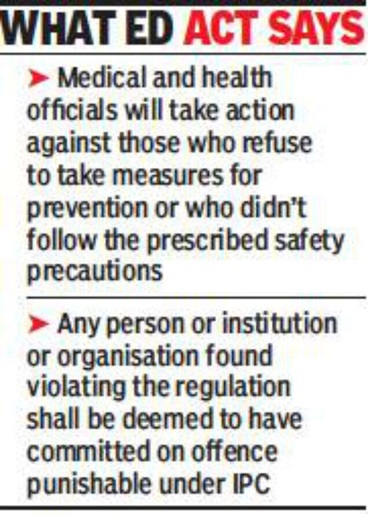
Description of the Epidemic Diseases Act, 1897
The Epidemic Diseases Act was passed in 1897 with the aim of
better preventing the spread of “dangerous epidemic diseases”
It evolved to tackle the epidemic of bubonic plague that
broke out in the then Bombay state at the time.
- The Epidemic Diseases Act is one of the shortest Acts in India, comprising just four sections.
- The first section explains the title and the extent,
- while the second gives powers to the state and central governments to take special measures and formulate regulations that are to be observed by the people to contain the spread of disease.
- The third section describes penalties for violating the regulations, in accordance with Section 188 of the Indian Penal Code.
- The fourth deals with legal protection to the implementing officers acting under the Act .
Three key measures
- “Test, trace and isolate”
- Testing and quarantine;
- Changes in behaviour that reduce transmission (which include social distancing, the wearing of masks and hand washing);
- Targeted lockdowns of outbreak hotspots—a practice known as a “circuit-breaker”
Covid-19 FMGE Question
When did WHO declare Covid19 as Pandemic
R0 refers to
R0 of seasonal flu
Confirmed and suspected cases of 2019-nCoV infection should be entered onto the IDSP database within how many days
Median incubation period of COVID-19
Which of the following pairs are matched wrongly
Serial interval originated from with reference to which disease epidemic
Containment zone in an area refers to
Contact tracing is an example of
Targeted lockdowns of outbreak hotspots
To date, two diseases have been eradicated using herd immunity and vaccination: rinderpest and
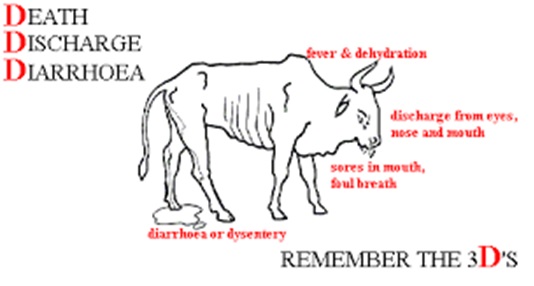
Rinderpest – also known as cattle plague – was a disease caused by the rinderpest virus which primarily infected cattle and buffalo. Infected animals suffered from symptoms such as fever, wounds in the mouth, diarrhea, discharge from the nose and eyes, and eventually death.
The rinderpest-free status would be applicable from November 1, 2004 in India.
On 28 June 2011 World was free of Rinderpest